Read on to find out more about the Pancreatic Stones Diet. Eating in a Pancreas-friendly way should be the aim of all. But if it's too late for that the Pancreatic Stones Diet is still your best option, as we explain below.
Recovering through your diet
A pancreas-friendly diet is high in protein from lean meats and low in animal fats and simple sugars, Dr. Chahal says.
You should eat plenty of:
- Vegetables
- Beans and lentils
- Low-fat or nonfat dairy (almond or flax milk).
- Antioxidant-rich foods such as dark, leafy vegetables, red berries, blueberries, sweet potatoes, grapes, carrots, walnuts, and pomegranates are also beneficial.
But, only eat avocado, olive oil, fatty fish, nuts, and seeds in moderation.
The Mediterranean diet is a good option for you if you are recovering from mild acute pancreatitis. You can find healthy recipes in the National Pancreas Foundation cookbook, Dr. Chahal says.
While receiving treatment for pancreatic cancer, it is likely your body will suffer nutritionally as it attempts to fight the cancerous cells in your body or recover from pancreas surgery.
For those receiving treatment for pancreatic cancer, or those recovering from the Whipple procedure or some other surgical treatment, here is a nutrition guide of foods to eat when you have pancreatic cancer so that you can maintain a strong body while fighting your illness.
Just make sure to discuss any special dietary needs with your pancreas surgeon to make sure you are maintaining optimal health post-treatment and receiving proper nutrition for pancreatic cancer. He or she can give you the most personalized idea about the best foods for pancreatic cancer.
Pancreatitis is both more common and more severe in the overweight. Inactivity may also be a contributor, so weight loss and exercise are both important. Many weight-loss diets are extremely high in carbohydrates, with low fat and low protein.
A low-fat diet is not required to lose weight, and higher protein helps lose fat, while low protein can lead to muscle loss. It’s in principle better to choose a diet that has higher protein and moderate amounts of fat and carbohydrates to lose weight.
Check Current Diet Book PricesWhat is the Best Diet for Pancreatitis?
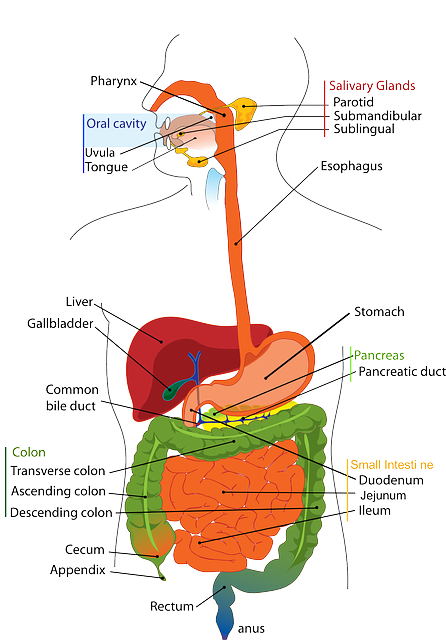
Your pancreas helps you regulate the way that your body processes sugar. It also serves an important function in releasing enzymes and helping you digest food. When your pancreas becomes swollen or inflamed, it cannot perform its function.
This condition is called pancreatitis. Because the pancreas is so closely tied to your digestive process, it’s affected by what you choose to eat. In cases of acute pancreatitis, pancreas inflammation is often triggered by gallstones. But in cases of chronic pancreatitis, in which flare-ups recur over time, your diet might have a lot to do with the problem. Researchers are finding out more about foods you can eat to protect and even help to heal your pancreas.
Chronic pancreatitis often has more severe symptoms. For this reason, more extensive treatments may be required, including one or more of the following:
- iv fluids, which may cause high blood pressure, fluid retention, kidney damage, electrolyte imbalances, and even heart failure.
- Pain medications, which may lead to constipation, drowsiness, and nausea, and may be habit-forming.
- Dietary changes to a low-fat diet with easily absorbable proteins, which may result in weight loss.
- Dietary enzymes, which may cause upset stomach, gas, headaches, constipation, sore throats, cough, ear pain, heartburn, and nosebleeds.
If you have symptoms of an allergic reaction, you should call your doctor immediately.
In cases of mild pancreatitis, enteral nutrition should be recommenced as soon as abdominal pain has subsided. In severe pancreatitis, patients should be kept nil by mouth until fully resuscitated, usually after 48 hours, at which point normal enteral diet (if tolerated) or enteral tube feeding should be commenced.
Meta-analyses have demonstrated that enteral nutrition, compared with parenteral nutrition, decreases sepsis, organ failure, the need for surgical intervention and mortality.
Post-pancreatic feeding is no longer recommended unless there is mechanical gastric outlet obstruction or the patient is unable to tolerate nasogastric tube feeding.
Parenteral nutrition should be reserved for patients who are unable to reach nutritional goals with nasojejunal feeding. A delay of up to 5 days in the initiation of parenteral nutrition may be appropriate to allow for restarting of oral or enteral feeding. Pancreatic enzyme supplementation should be prescribed to patients with symptoms of pancreatic exocrine insufficiency.
Is There a Specific Diet for Pancreatitis?
Pancreatitis occurs when the pancreas becomes inflamed and the digestive enzymes that should only be active inside the intestines start “digesting” the pancreas itself.
This condition can not only be painful but also interfere with your digestion and prevent food from being properly absorbed, which can lead to nausea, vomiting, bloating fever, and diarrhea. As a result of pancreatitis, you can develop serious nutritional deficiencies and lose weight.
Pancreatitis can be acute (meaning it occurs suddenly) or chronic (i. e. long term). In most cases, acute pancreatitis goes away in a few days with specific dietary changes or treatments, which may include fluids, antibiotics, or pain medication. Inflammation of the pancreas that gets worse over time is considered chronic pancreatitis.
Persistent or chronic pancreatitis can damage the pancreas and lead to other problems, such as epi, which develops when the pancreas isn’t able to produce the digestive enzymes needed to digest food.
While the specifics of a pancreatitis diet plan will depend on your dietary needs and preferences, there are some general guidelines you can use as a starting point. It’s generally recommended that you avoid choices that are:
- high in fat
- have a lot of sugar
- contain alcohol.
The guidelines for fat intake if you have pancreatitis vary. For example, the digestive health center at Stanford University recommends patients with chronic pancreatitis limit fat intake to 30 to 50 grams per day, depending on how well it’s tolerated.
Check Current Diet Book PricesDiet Chart For acute pancreatitis
When it comes to pancreatitis patients, nutrition is very crucial. To recover and avoid pancreatitis-triggered diseases like gallstones, pancreatic cancer, diabetes, and malnutrition, patients must follow a good diet. Here’s an acute pancreatitis diet chart – take a look.
:max_bytes(150000):strip_icc():format(webp)/2507165-article-diet-and-chronic-pancreatitis-5a5e6e3996f7d00037173956.png)
Malnutrition diabetes along with diet and lifestyle changes, you must also be aware of other treatments available for pancreatitis.
Pancreatitis Diet Tips for Prevention & Management
Nearly 300,000 people are admitted to the hospital for pancreatitis each year in the United States alone. This is a very serious and painful condition that requires careful medical observation. In fact, during the first few days, no food or liquid is allowed; all fluids are administered through an iv.
As the pancreas begins to heal and function once again, first clear liquids are allowed, and then bland, low-fat foods are added under the watchful eye of the health care team to make sure that food is well-tolerated. Acute pancreatitis can be life-threatening; seeking medical treatment is a must.
Treatment of chronic pancreatitis emphasizes the prevention of additional pancreatic injury, pain relief, nutritional support, and replacement of lost endocrine/exocrine function.
To achieve this, alcohol must be completely removed from the diet of those with alcohol-related pancreatitis, and smoking should be avoided, as it has been associated with a greater risk of mortality in people with alcohol-related pancreatitis.
The pain associated with this disease can be treated with nonnarcotics in the early phases of the disease with a progression to narcotics as the disease develops and the pain becomes more chronic.
However, there is a 10% to 30% risk of addiction for those patients with chronic pancreatitis who are using narcotics for pain relief. In addition to these drugs, high-dose pancreatic enzyme therapy is effective at reducing pain in patients with small duct disease, but not large duct disease, while nerve blocks can also facilitate pain relief.
Also, an h2 blocker or proton pump inhibitor may be used to reduce the acid-stimulated release of secretin and, therefore, the circulation of pancreatic enzymes. Pain directly associated with pancreatic structural changes or complications may be treated in different ways.
Check Current Diet Book PricesPancreatitis Diet – Foods To Eat And Avoid And Lifestyle To Follow
Avoid hamburgers, pizza, fries, and fried chicken. Also, steer clear of cake, pastries, doughnuts, ice cream, and milkshakes. It is clear that you must avoid foods that are unhealthy and make your digestive system work extra hard to help digest them.
Make sure you consult your doctor before you decide to follow a diet plan.
Pancreatitis Diet – Foods To Avoid
Nutrition is a vitally important part of treatment for patients with pancreatitis. The primary goals of nutritional management for chronic pancreatitis are:
- prevent malnutrition and nutritional deficiencies
- maintain normal blood sugar levels (avoid both hypoglycemia and hyperglycemia)
- prevent or optimally manage diabetes, kidney problems, and other conditions associated with chronic pancreatitis
- avoid causing an acute episode of pancreatitis
- to best achieve those goals, it is important for pancreatitis patients to eat high protein, nutrient-dense diets that include fruits, vegetables, whole grains, low-fat dairy, and other lean protein sources. Abstinence from alcohol and greasy or fried foods is important in helping to prevent malnutrition and pain.
Unfortunately, it is not possible to be 100% sure you will prevent gallstones from forming, and pancreatitis caused by that. The good news is that you can take steps to reduce the risk factors for this condition. These include:
- A healthy diet – try to avoid unhealthy and processed foods, especially those meals loaded with fat. Maintain optimal weight – obesity might be a risk factor for gallstones.
- Maintain optimal blood sugar and cholesterol levels – diabetes and increased cholesterol might add to the risk of developing gallstones.
There are ways you can protect your pancreas and reduce your risk for pancreatitis and other serious health problems such as epi.
1. Limit alcohol consumption. By drinking less (or not at all), you can help protect your pancreas from the toxic effects of alcohol and reduce your risk for pancreatitis.
2. Eat a low-fat diet. Gallstones, a leading cause of acute pancreatitis, can develop when too much cholesterol accumulates in your bile, a fluid that helps break down fats. To reduce your risk for gallstones, eat a low-fat diet that includes whole grains and a variety of fresh fruits and vegetables.
To help prevent pancreatitis, avoid fatty or fried foods, and full-fat dairy products.
Check Current Diet Book PricesHealthy Gallbladder Foods
Maintaining a healthy diet and weight go a long way in keeping the gallbladder healthy. “you should eat a well-balanced diet with fruits, veggies, lean meats, and fiber,” advised Knowlton. According to a new health guide, foods that are particularly good for the gallbladder are:
- Fresh, fiber-rich fruits and vegetables: some great ones are avocados, cranberries, berries, grapes, cucumbers and beets.
- Broccoli, bell peppers and oranges are high in fiber and vitamin c, which if lacking can contribute to gallstones.
- Pectin-rich fruits — such as apples, strawberries and citrus — can also help.
According to rawpeople. Com. Radishes are a terrific option because they increase bile flow, but those already suffering from gallbladder problems shouldn't eat too many of them.
Diet for a healthy gallbladder
A high fiber diet appears to reduce the chance of gallstone formation. Soluble fiber from grains and other foods is believed to lower the blood cholesterol level. Oats and barley are good sources of this type of fiber.
Several research studies have discovered that drinking caffeinated coffee regularly and ingesting vitamin C seems to reduce the risk of gallstone formation. Scientists are not ready to make definite claims that certain foods or nutrients are beneficial for the gallbladder, however. It's always good to follow a healthy diet.
It's important to keep in mind that ingesting a particular food or drink in excess or taking an excessive dose of a vitamin supplement may be harmful, however. Questions about the best diet to follow with respect to gallstones should be referred to a doctor.
About 40 percent of pancreatitis cases are related to gallstones, according to the University of Maryland medical center. The gallstones cause inflammation in the pancreas as they pass through the bile duct. Gallstones are small pebbles formed in the gallbladder.
In the hospital, a person with gallstone-related pancreatitis may not be allowed to eat. Once discharged to home, you will be advised to follow a low-fat diet.
Total fat intake for pancreatitis and gallstones is usually limited to 20 percent of total calorie intake, according to the Jackson/Seigelbaum gastroenterology group.
Most bread and grains are naturally low in fat and are healthy diet food choices for people with pancreatitis and gallstones.
You will need four or more servings of bread and grains a day.
Choices include whole-wheat bread and bread products, plain pasta, plain rice, whole-grain cereals, saltine crackers, soda crackers, oatmeal, rice cakes, air-popped popcorn, low-fat muffins, pancakes made without added fat and french toast made with skim milk and egg substitute.
Check Current Diet Book PricesLow-fat Diet
Always check with your doctor or dietician before changing your eating habits when you have pancreatitis. Here are some tips they might suggest:
- eat between six and eight small meals throughout the day to help recover from pancreatitis. This is easier on your digestive system than eating two or three large meals.
- Use Mcts as your primary fat since this type of fat does not require pancreatic enzymes to be digested. Mcts can be found in coconut oil and palm kernel oil and is available at most health food stores.
If you’re diagnosed with acute pancreatitis, you should stop drinking and eat a low-fat diet. This will reduce your risk of another attack and developing chronic pancreatitis. If you develop chronic pancreatitis your pancreas will stop working properly.
The outlook for most cases of chronic pancreatitis is not good. The damage is irreversible and you’ll need to go on permanent medication to help you digest food and to maintain blood sugar levels. It’s a painful condition, but in many cases, after years of treatment, the pain improves or sometimes disappears.
With the removal of large portions of your pancreas during the Whipple procedure, pancreatic enzymes that are normally produced to aid in the absorption of fat, proteins, and carbohydrates during the digestive process may no longer be produced.
The result is poor nutrition and can lead to malnutrition quickly. Here is a breakdown of the pancreatic enzymes necessary for digestion that may need to be supplemented into your post-Whipple diet:
lipase – working with the bile produced via the liver, lipase breaks down fat molecules to be absorbed and used by the body for energy. Lack of fat absorption results in the body’s inability to absorb fat and fat-soluble vitamins needed by the body, such as vitamins E, S, A, and K.
Oxalate and a Vegetarian Diet
A 2014 study from epic-oxford measured the risk of being hospitalized for a kidney stone over the course of five years for people in various diet groups. Vegetarians (including vegans) had a 31% lower risk (. 69. 48–0. 98) as compared to high meat-eaters.
While people who have had calcium-oxalate kidney stones need to watch their oxalate intake, the evidence that a diet moderately high in oxalate puts the average person at risk for kidney stones is not strong. The health professionals follow-up study (hpfs) and the nurses’ health studies i and ii are two of the largest and best designed prospective studies on nutrition and health. In 2007, they reported an increased risk of kidney stones for men between the highest one-fifth of oxalate intake (median of 328 mg/day) compared to the lowest one-fifth (median of 106 mg/day) of 1. 22 (1. 03- 1. 45). For older women, the risk for the highest one-fifth (median of 287 mg/day) compared to the lowest one-fifth (87 mg/day) was 1. 21 (1. 01-1. 44). There was no association for younger women.
If it's a fibrocystic disease, you cannot do much about it since it's typically not a disease. To rule out any cancer risks, regular physical breast exams and mammograms are important. Limiting or avoiding caffeine is also suggested, especially when it comes to managing the pain due to fibrocystic breast. Some women discovered that chocolate worsens the pain. Because of this, people have to pay more attention to what they eat. They have to check which foods or drinks cause more pain. A good rule of thumb to follow is to lower salt consumption, as it also helps to reduce any swelling. A high-fiber, low-fat diet will help lower the risk of developing cancer.
If you've been diagnosed with chronic pancreatitis, it has been said that you should be offered:
- annual checks (every 6 months in under-16s) to make sure your diet is giving you the nutrients you need a bone density assessment every 2 years – problems with digesting foods may affect your bone health
- a blood test for diabetes every 6 months
- an annual check for pancreatic cancer if the cause of chronic pancreatitis is hereditary.